
Ashley worked as a chef before COVID-19 hit. As a result of the pandemic, she lost her job and her health insurance — a plight an estimated 20 million Americans also faced.

Ashley worked as a chef before COVID-19 hit. As a result of the pandemic, she lost her job and her health insurance — a plight an estimated 20 million Americans also faced.
In this digital version of the 2021 Medication Access Report, hear from patients struggling to get the medications they need, review data on major medication access challenges and discover healthcare solutions that can make a difference.
For a deeper look into the data driving this year's report, download the full 2021 Medication Access Report.
Editor: Patient last names have been omitted to protect their privacy.
Ashley and her wife moved to Georgia in February 2020 so she could take a new job. She had recently been diagnosed with fibromyalgia and finally found a drug that helped effectively manage the major depressive disorder she also lives with.
Then COVID-19 hit.
Ashley became one of the estimated 20-million Americans who lost their jobs as well as their health insurance.COVID-19 and Medication Access, CoverMyMeds, 2020
Without health insurance, she could no longer afford her medications: Her prescription for depression alone was around $1,700 a month. While her doctor worked with her to find affordability options, each visit cost her nearly $200, even for telehealth.
“It’s been difficult to manage because there’s not really a need to go to an appointment if I can’t afford the medicine she’s going to write the prescription for,” Ashley said.

Without income or insurance, Ashley had to manage her fibromyalgia pain and major depressive disorder without prescription medications. Some days she could barely make it out of bed.
Ashley can relate to the 36 percent of patients surveyed who have given up their medications to help pay for life’s essentials.CoverMyMeds Patient Survey, 2020 Others have done the inverse: Forty-three percent said they’ve had to forgo paying for essential items and bills to afford their medications.CoverMyMeds Patient Survey, 2020 Some try to make both work: Forty-one percent said they’ve skipped or modified medication doses to stretch out their prescription.CoverMyMeds Patient Survey, 2020

To ease her fibromyalgia pain while job searching, Ashley took 800 mg of ibuprofen just to get out of bed each day. Her depression went unmanaged.

Ashley fell back on over-the-counter drugs to relieve her pain and energy drinks to combat fatigue so she could search for a job to regain health insurance.
“Situational depression from (COVID-19), on top of not-having-employment depression, on top of the fibromyalgia-related depression has caused a spiral in stress and anxiety that I have never felt before,” Ashley said. “I’ve had debilitating anxiety just worrying about where our next meal is going to come from.”

While 63 percent of providers surveyed said income level affects their patients’ ability to access healthcare, only 17 percent are asking patients about their household income.CoverMyMeds Provider Survey, 2020 This layer of personal insight combined with point-of-prescribing solutions such as real-time prescription benefit (RTPB) could help prescribers open the door to pivotal patient affordability conversations.

Ashley and her wife had to make careful financial decisions as they managed life on little to no income, stretching out food stamps each month.
In October 2020, after seven months without her medications, Ashley finally got a job that offered health insurance. The first things she did were schedule a surgery her wife had put off and checked the price of her medications.
“Everything is going to slowly fall back into place,” she said. “(Health insurance) takes a weight off — a weight that I can’t even describe.”

Ashley and her dog, Samoa, take a walk in her small Georgia town, a feat she now accomplishes with much less pain since being able to afford her medications again.
Unfortunately, insurance coverage isn’t always the key to affordability, especially since high deductible health plans encompass 46 percent of employer-based insurance plans for those under 65 and 90 percent of Affordable Care Act exchange programs.Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey, January–September 2018, National Center for Health Statistics, 2019 Patients on these plans carry the load of paying for their medical expenses most of the year — if not all of it.

Discover more data-driven insights and analysis in this year's full report — including how healthcare technology can help mitigate industry-wide affordability barriers. Download the full 2021 Medication Access Report.

Tonia is a single mother and caregiver to her active teenage son.
Tonia is a single mother to an active 14-year-old son. A couple years ago, he started losing patches of hair. They also noticed his fingernails starting to discolor and become brittle, “like broken glass,” Tonia said. They were so fragile they would often rip off completely and bleed from getting snagged on a shirt.
His doctor diagnosed him with pediatric psoriasis and alopecia. While she grappled with knowing her son had a chronic condition with no known cure, she was relieved to hear there was a treatment to improve his symptoms. Tonia expected to visit the pharmacy, pay for and pick up the medication and go home to start treatment with her son. Unfortunately, that would not be the case.

Tonia's son smiles at his reflection in the mirror after a fresh haircut. His barber takes special care to hide any bare spots caused by alopecia.
The pharmacist told Tonia her insurance plan required a prior authorization (PA) before she could start her son’s medication. While they went home and waited for the PA to be approved, Tonia described herself as a "nervous wreck.”
“When the medication for my son was denied, it was really disappointing, disheartening to know I wouldn't be able to go home and start the treatment process with my son,” Tonia said. “My son felt sad, defeated, frustrated, discouraged."

After learning her son's medication would require a PA, Tonia spent time on the phone with her insurance plan and provider trying to find answers.
Tonia's story is not unique. Delays in care due to traditionally manual and multi-step benefit processes are some of the most common medication access challenges patients face. One in four patients surveyed reported a delay in receiving their medication due to PA.CoverMyMeds Patient Survey, 2020

Providers are frustrated, too. Most listed PA requests as a time-consuming part of their workday, and over half indicated they don’t have enough time to complete them.CoverMyMeds Provider Survey, 2020 Because of PA management, over one third of providers had less time for face-to-face interaction with patients — during which affordability and access conversations could occur.CoverMyMeds Provider Survey, 2020

Like many families this year, Tonia and her son adapted to working, learning and managing their health remotely.
Tonia expressed what many caregivers feel when trying to manage medication access — that she’s coming up short for her son.
“It's frustrating because you think, if anything, we should all be on the same team and the goal should be to let everyone receive the medication they need, but unfortunately, for whatever reason, it's not the case,” Tonia said.

Tonia and her son joke as they walk off the field after throwing the football. Finding ways to help manage the PA process can help patients get back to living healthy, active lives.
Initiating PA requests at the point of prescribing could reduce administrative burden for pharmacists and for providers later on in the process. But fewer than one in five providers do so, most waiting for the pharmacy to notify them of prior authorization requirements.CoverMyMeds Provider Survey, 2020 More than half of pharmacists surveyed reported spending at least an hour on insurance-related rejections each day, with one in five spending two or more hours daily on these tasks.CoverMyMeds Pharmacist Survey, 2020 When a PA request is submitted prospectively, at the point of prescribing, patients access their medications about 13 days sooner, on average.CoverMyMeds data on file, 2018

Integrated solutions within a provider's workflow can help speed up the PA process. Nearly all respondents are using an electronic method, and adoption of ePA increased 13 percent over last year's provider survey. CoverMyMeds Provider Survey, 2020,CoverMyMeds Provider Survey, 2019 Still, over half of providers said they are using fax to submit at least some PA requests. Nearly half are still using the phone, numbers that have remained steady over the past two years.CoverMyMeds Provider Survey, 2020,CoverMyMeds Provider Survey, 2019 Lack of interoperability between electronic systems and cost are some of the reasons these manual methods persist, decades after most industries have moved on from the fax machine.Why Your Doctor's Office Still Depends on a Fax Machine, Stanford School of Medicine, 2019 When a PA request is submitted electronically, patients can get their medication faster and are more likely to adhere to their prescribed therapy.CoverMyMeds data on file, 2019

Tonia pulls away from the pharmacy after picking up her son's prescription.
While costs and administrative processes can be obstacles at the pharmacy counter, other variables can also affect patients medication access. Social determinants of health — such as socioeconomic status, education, transportation options, physical living environment, race and ethnicity — have always affected healthcare, but many entered the forefront in 2020. Taking action on them may be the catalyst in shifting the healthcare industry's view from patients to people.
When surveyed, minority patients were more likely than average to be affected by finances, stretch out medication doses and make difficult decisions between their treatment and paying for essential items.CoverMyMeds Patient Survey, 2020 Three-fourths of minority patients surveyed were financially affected in some way by COVID-19 compared to just over half of white patients.CoverMyMeds Patient Survey, 2020

While many racial disparities can be linked to financial concerns, studies showed even Black Americans with high incomes and socioeconomic status are less protected from chronic medical conditions than whites of the same status.The Benefits of Higher Income in Protecting against Chronic Medical Conditions Are Smaller for African Americans than Whites, Assari, 2018 Even technology algorithms can’t always factor out the complex issue of racial bias.Dissecting Racial Bias in an Algorithm Used to Manage the Health of Populations, Obermeyer, Powers, Vogeli, Mullainathan, 2019
Race and ethnicity are among many variables to consider in healthcare technology — which is why it’s important for providers to bring the human lens to patient interactions. When deciding on the best path to medication access, providers have the opportunity to consider all variables that could impact each patient individually. Yet, one in five providers surveyed said they aren’t asking patients about social determinants of health.CoverMyMeds Provider Survey, 2020
Go deeper into this year's full report to discover more data-driven insights and analysis — including how social determinants of health impact medication access. Click here to download the full 2021 Medication Access Report.

Chronic conditions can force difficult decisions. For Michael, scleroderma eventually caused him to leave his thriving career.
Michael still holds the record for most cars sold in a single month at the rural Michigan dealership where he last worked seven years ago: twenty-nine, if you were curious.
“That’s pretty good at any size dealership,” he said.
He was the top salesman and finance director of the family-owned dealership in his town of 5,000 people. At 55 years old, he was putting in over 60 hours a week when he started showing symptoms of what he would soon learn was scleroderma, an autoimmune disease that affects connective tissue. Despite trying to work through the condition, Michael was forced to retire.
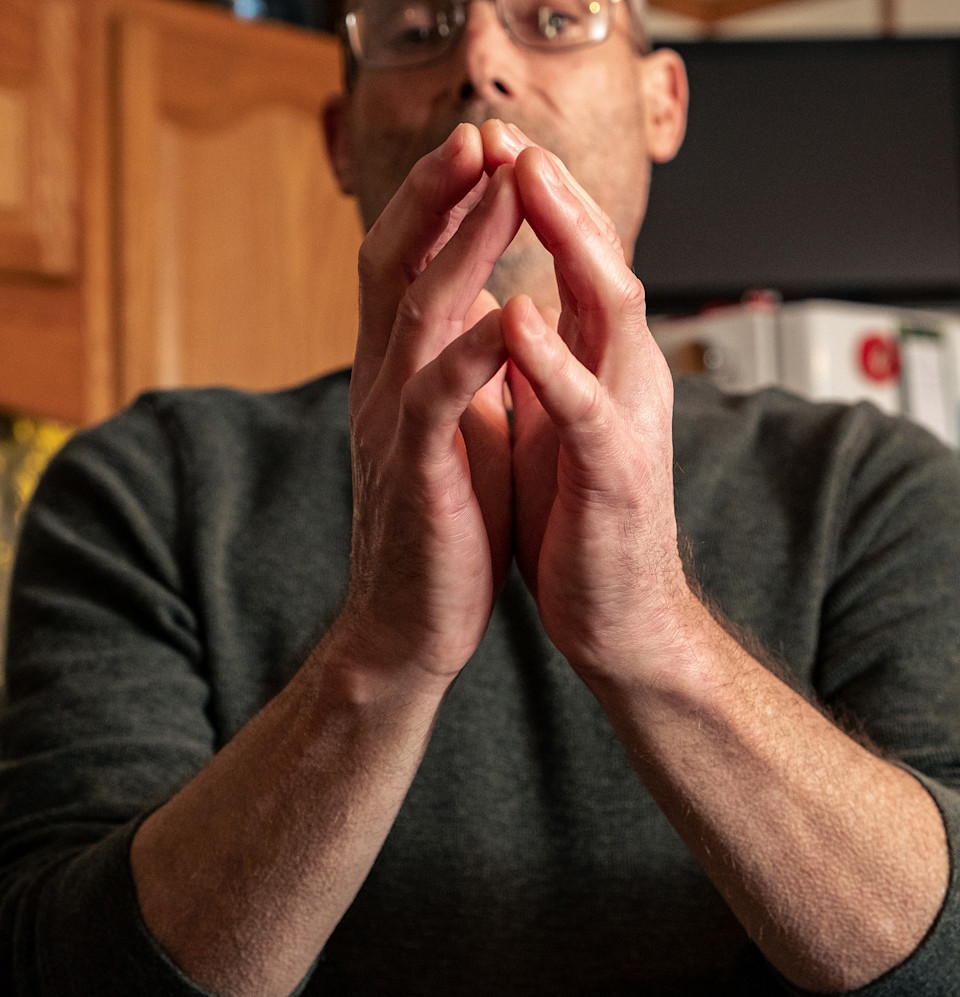
Michael displays the swelling, thickened skin on his hands, one of the earliest, often painful, symptoms of scleroderma.
“I was a million-dollar seller,” he said. “With scleroderma I could not keep up; the fatigue became phenomenal. There was no way I could work those hours. I tried.”
Michael had trouble finding a good rheumatologist near his rural town. The provider he finally found was located two hours away in Ann Arbor. While telehealth was an option, Michael preferred face-to-face appointments, especially since scleroderma affects the skin, making examinations difficult over video calls. Internet connectivity issues and the impersonal feeling of virtual interactions added to his dislike for telehealth.

After finding few support groups for his condition, Michael started his own — and now manages a full schedule of patient advocate work.
An online healthcare aspect Michael does appreciate are virtual patient support groups. While finding a scleroderma, or even a general patient advocacy group, would be a tall order in his area, Michael has been able to connect with other patients around the globe through social media. They discuss symptom management, medications and other hurdles to chronic conditions such as insurance authorizations, affordability and provider access. Michael leads many of the groups and even leads online webinars to help patients find the right path to disease management.
“There are ways to navigate the system, but most people, when they’re fighting a disease that they can’t even get out of bed with some days and don’t have the stamina, they lose the will to fight, they give up,” Michael said. “And I don’t want anyone to give up. I want to help people.”

Michael has learned what tools he needs to manage his condition daily — even when his provider is a two-hour drive from his rural town.
Fewer than one in three providers surveyed said they ask patients about their access to technology and mass media.CoverMyMeds Provider Survey, 2020 But nearly half said it’s a factor that impacts their patients’ ability to access healthcare; the same number indicated patients’ skill level with technology impacts healthcare access.CoverMyMeds Provider Survey, 2020

Michael takes a break from yardwork, a chore he can continue to do with his condition managed through a combination of technology, medication and the right support team.
A social determinants of health screening could identify patient technology disparities — especially important as telehealth use has ramped up. This information, integrated into EHR and patient-accessible portal data, could help physicians make better prescribing decisions. This easy-to-access prescription decision technology, inclusive of RTPB and ePA, can continue to support providers for their patients who choose telehealth to expedite appointments and improve medication adherence.
Press inquiries:
media@covermymeds.com
The Medication Access Report is developed in consultation with an advisory board of healthcare experts representing major organizations across the industry — each with unique perspectives, interests and opinions.